Ranibizumab
What is Lucentis (Ranibizumab)?
Approved To Treat
Related Clinical Trials
Summary: This study will evaluate the efficacy, safety, and PK of ranibizumab 100 milligrams per milliliter (mg/mL) delivered every 24 weeks (Q24W) via the PDS implant compared with ranibizumab 0.5 milligrams (mg) delivered every 4 weeks (Q4W) as intravitreal (IVT) injection in chinese participants with nAMD.
Summary: This study will evaluate the long-term safety and tolerability of the Port Delivery System with ranibizumab (PDS) (100 mg/mL) in participants with neovascular age-related macular degeneration (nAMD) who have either completed Phase II Study GX28228 (Ladder), Phase III Study GR40548 (Archway), Phase IIIb Study WR42221 (Velodrome), or completed Week 24 visit in Study WR42221 but were not eligible to ...
Summary: This study will assess corneal endothelial cells in participants with nAMD treated with PDS refilled every 24 weeks (Q24W).
Related Latest Advances
Brand Information
- Colorless to pale yellow 10 mg/mL solution (LUCENTIS 0.5 mg)
- Colorless to pale yellow 6 mg/mL solution (LUCENTIS 0.3 mg)
- Endophthalmitis and Retinal Detachments
- Increases in Intraocular Pressure
- Thromboembolic Events
- Fatal Events in patients with DME and DR at baseline
- Ocular: Tear of retinal pigment epithelium among patients with neovascular AMD
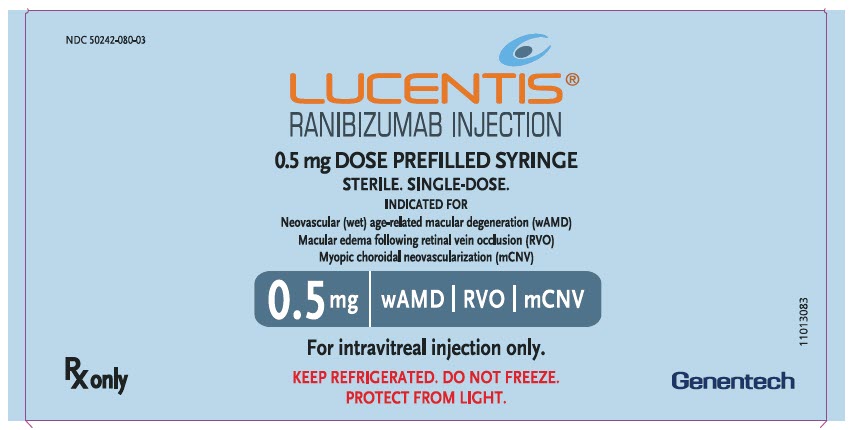
- Each LUCENTIS 0.5 mg carton (NDC 50242-080-03) contains a single-dose, prefilled syringe designed to deliver 0.05 mL of 10 mg/mL ranibizumab solution. The prefilled syringe has a non-retractable plunger stopper and a syringe cap consisting of a tamper-evident rigid seal with a rubber tip cap including a Luer lock adapter. The prefilled syringe has a plunger rod and a CLEAR finger grip. Each prefilled syringe is sterile and is packed in a sealed tray.
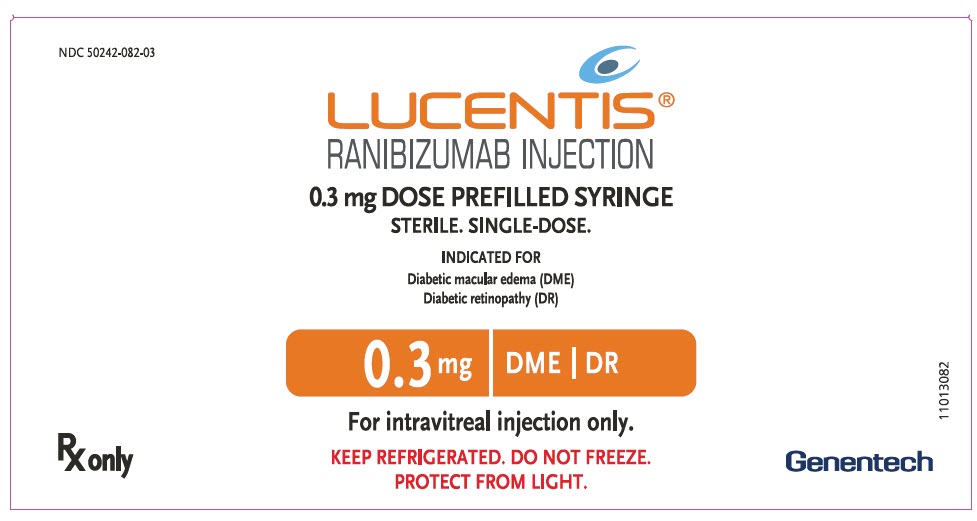
- Each LUCENTIS 0.3 mg carton (NDC 50242-082-03) contains a single-dose, prefilled syringe designed to deliver 0.05 mL of 6 mg/mL ranibizumab solution. The prefilled syringe has a non-retractable plunger stopper and a syringe cap consisting of a tamper-evident rigid seal with a rubber tip cap including a Luer lock adapter. The prefilled syringe has a plunger rod and an ORANGE finger grip. Each prefilled syringe is sterile and is packed in a sealed tray.